

The majority of patients had hypertension (73%) and hyperlipidemia (50%). Low risk was defined as having a score 48 h (n = 15, 6%) or unknown (n = 30, 12%) for the remaining patients. Patients' ABCD 2 scores were dichotomized into low risk and high risk.
#Abcd 2 score plus#
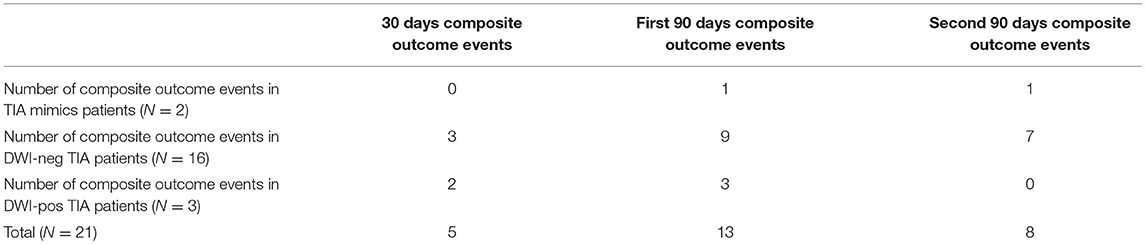
In-hospital intervention plus in-hospital ischemic events were combined to form a composite risk in order to more fully understand events following the index symptoms. heparin, warfarin, or novel anticoagulants). Anticoagulation was defined as initiation of intravenous or oral anticoagulation during hospitalization or at discharge (i.e. Revascularization of symptomatic arterial stenosis was defined as either endarterectomy or angioplasty/stenting of an extracranial internal carotid artery or angioplasty/stenting of an intracranial artery. intra-arterial lytic or mechanical embolectomy) was ascertained.
#Abcd 2 score Activator#
In-hospital use of intravenous tissue plasminogen activator and/or endovascular reperfusion therapy (i.e. Secondary outcome measures included all in-hospital intervention as detailed below. Patients were considered to have had an ischemic stroke if follow-up MRI or CT confirmed new areas of ischemia not previously present, with persistent clinical symptoms lasting >24 h and to have recurrent TIA if symptoms lasted ≤24 h. The primary outcome measure was in-hospital ischemic events, defined as a return of previously resolved symptoms or new focal neurological symptoms.
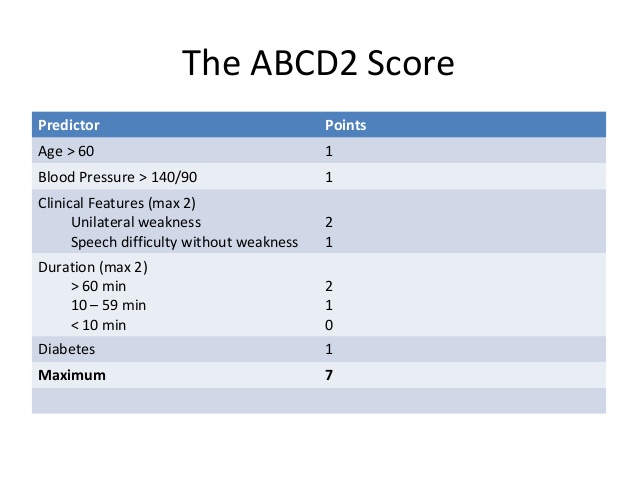
Patients initially admitted for possible TIA but later determined to have an alternate diagnosis were excluded from our study. An ABCD 2 score was calculated for each patient by the primary study physician based on clinical data available in the patient's chart. Methods: We reviewed consecutive patients admitted between 20 following a TIA, defined as transient focal neurological symptoms attributed to a specific vascular distribution and lasting 50% stenosis on the symptomatic side. We aimed to determine if there is a relationship between ABCD 2 scores, in-hospital ischemic events, and in-hospital treatments after TIA admission. The American Heart Association recommends admission of patients with ABCD 2 scores ≥3 for observation, rapid performance of diagnostic tests, and potential acute intervention. Background and Purpose: Following transient ischemic attack (TIA), there is increased risk for ischemic stroke.


 0 kommentar(er)
0 kommentar(er)
